During pregnancy, most expecting women anticipate common discomforts like weight gain, swollen feet or fatigue. Yet despite an estimated 33% experiencing urinary incontinence after birth, lack of awareness leaves many shocked by sudden leaks and loss of bladder control postpartum.
Postpartum bladder changes arise primarily due to stresses placed on pelvic floor muscles during pregnancy and delivery. Pressure from the baby’s head and intense pushing during labor stretch tissues and nerves supporting bladder control. Delivering multiple children or an exceptionally large infant further increases risks.
For over 80% of new mothers affected, symptoms persist for up to a year but eventually resolve within five years. Yet for 1 in 3 women, postpartum issues become a lifelong condition without proper treatment.
Incontinence supplies provide practical protection when leaks occur. Yet many women hesitate to discuss this sensitive issue, even among loved ones or doctors. Letting fear of stigma keep you from seeking solutions leads to unnecessary discomfort and isolation.
Decoding the Different Types of Urinary Incontinence
Categorizing the type and circumstances around your incidents leads to more targeted solutions. Here are some of the common types of incontinence following childbirth:
- Stress Incontinence- The most prevalent form for new moms involves leaks when pressure acts on an overstretched bladder, like sneezing or lifting.
- Urge Incontinence – Defined by abrupt, intense urges to empty the bladder followed by uncontrolled release.
- Mixed Incontinence – Many women experience both stress and urge types simultaneously following childbirth.
- Overflow Incontinence – Women who deliver via complex C-sections more often suffer from overflow incontinence due to nerve damage affecting bladder signals.
Psychological Impact
Coping with unpredictable bladder leaks causes much more than just physical annoyance for new mothers. The effort involved in constant vigilance around triggers leads to anxiety and overwhelm trying to prevent leak accidents.
Mothers describe a constant daily preoccupation about when another public accident might happen. The effort involved in scanning for bathrooms, avoiding triggers, and hiding stains under baggy clothing causes exhaustion. It also leads many mothers to turn down social events and isolate themselves out of fear.
New research also illuminates emotional and psychological correlates as well. Mothers report that persistent incontinence causes them to lose self-confidence and negatively impacts their self-image over time. The stigma around adult leakage leads many women to have negative feelings, even though the loss of bladder control after the trauma of childbirth proves extremely common.
Furthermore, there are connections between chronic postpartum bladder issues and reduced relationship satisfaction. New mothers already grapple with fractured intimacy and changing marital dynamics. When the unreliability of incontinence gets added in, couples may drift further apart. Pelvic pain and sexual dysfunction frequently accompanying postpartum leakage contribute toward emotional distance as well.
Yet even despite how ubiquitous bladder control challenges prove for new mothers, social taboos keep the majority from ever discussing concerns openly with care providers or loved ones. Many suffer in silence rather than asking for help managing symptoms or accessing the necessary pelvic floor therapy. As stigma gets challenged through awareness and education, more women can seek solutions and are embracing incontinence underwear and other mitigation measures.

Seeking Help: Diagnosis Leading to Solutions
Since most postpartum bleeding and superficial first-degree tearing resolve within six weeks, many women wrongly assume ongoing leaks simply reflect slow individual recovery. Yet, leakage continuing longer than 10-12 weeks nearly always indicates a need for thorough expert pelvic floor assessment and proactive rehab-based treatment.
If you still experience unpredictable bladder leakage three months after delivering, make checking in with women’s health providers part of new mom self-care. Obstetrics, midwifery practices, and urogynaecology offer compassionate exams assessing contributing factors and guiding individualized treatment without shame. Come mentally prepared to share specific circumstances like activity levels, triggers and volume of accidents. This mapping illuminates the why behind leaks better than simply reporting frequency.
Today’s postpartum care experts aim treatment plans first at stopping uncontrolled symptoms at the moment while also teaching preventative techniques to avoid future recurrence after healing. They want every new mother to move positively forward, embracing parenting rather than hiding bladder challenges.

Recommendations span six fronts with high collaborative success rates:
1. Pelvic Floor Physical Therapy
Beyond traditional Kegels, today’s specialized pelvic physical therapists assess unique nerve and muscle injury patterns by charting personalized regenerative programs. Blending targeted massage, biofeedback and neuromuscular electrical stimulation, certified therapists quite literally reshape and heal damaged connective structures.
2. Bladder Retraining
Strategically timing bathroom breaks trains nerves and muscles to “relearn” coordinated communication rhythms. The bladder adapts capacity by proactively scheduling trips to empty every 1-3 hours (not waiting for urges) while preventing uncontrolled overflow accidents. This proven tactic empowers freedom from minute-to-minute worrying about leaks.
3. Hormonal Therapies
Seeking hormone balance through oral supplements, vaginal estrogen creams or pellet implants alleviates many cases of urge and stress incontinence. While not fully understood, these therapies help strengthen and support pelvic ligaments while regulating spasmodic signals. Combined with exercise plans, hormones provide temporary relief, allowing vigorous rebuilding.
4. Medical Devices
From simple silicone pessaries providing mechanical bladder support to mid-urethral slings incorporating mesh strips reinforcing weakened pelvic ligaments, specialty nurse practitioners today fit minimally invasive devices suited to each woman’s needs.
Unlike past surgical mesh debacles harming women, today’s refined precision devices bring non-surgical relief with lower risks. Still, expert fitting proves essential given anatomical complexities.
5. Surgical Intervention
Rarely indicated, mid-urethral slings incorporating mesh strips surgically reinforce actual weakened pelvic ligaments and muscles after more conservative treatments plateau or fail.
These outpatient procedures carry under 1 hour of recovery time with minimal impact on breastfeeding or parenting duties. While risks exist, state-of-the-art precision slings now help women permanently overcome even severe lifelong incontinence when led by specialist surgeons.
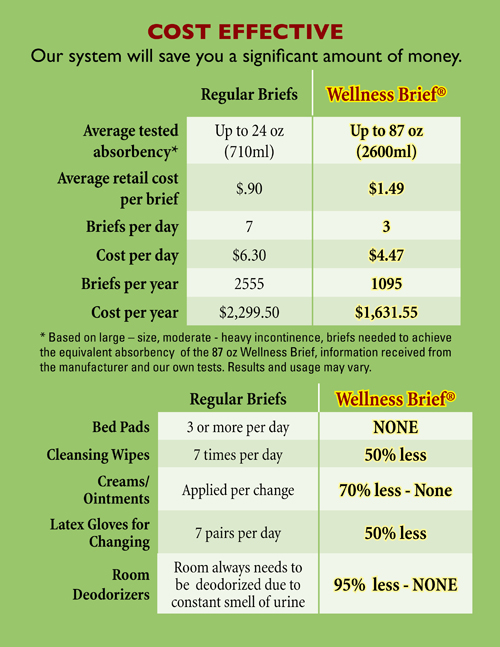
6. Absorbent Products
While pursuing proactive solutions, women’s incontinence underwear and absorbent pads discreetly save outfits and sanity during the postpartum phase. Stylish designs sit smoothly under clothing without awkward bulges, allowing new mothers peace of mind to cuddle infants without cringing over leaks. Sweat-wicking, quick-drying fabrics manage heavy surges, keeping skin dry for hours when needed.

Final Thoughts: Prioritizing Healing Starts with Support
Instead of resigning themselves to “acceptable losses,” new mothers embracing help beyond just hoping time alone fixes postpartum incontinence and reclaim vibrant wellness faster. Seeking diagnostic clarity and collaborating with aligned women’s health experts lead women to full recovery within a reasonable period.
Prioritizing pragmatic protection like adult incontinence products allows new mothers to focus energy entirely on nurturing babies rather than obsessing over unpredictable leaks. Combining proactive pelvic floor strengthening guided by compassionate specialists, women heal beyond postpartum bladder struggles too often borne silently out of persistent stigma.
When mothering young new lives, showing ourselves self-acceptance and patience using adaptive remedies proves just as vital as nourishing little ones. Continence concerns never define worthiness or completeness as mothers or women. So together, we help the next generation grow up knowing all bodies deserve respect and support rather than shame.


 `
`